

A co-pay maximizer program is one in which the amount of the patient’s out-of-pocket costs is adjusted to reflect the availability of support offered by a co-pay support program.
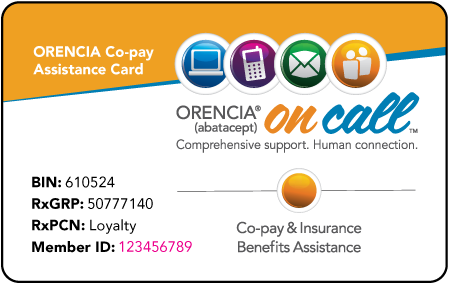
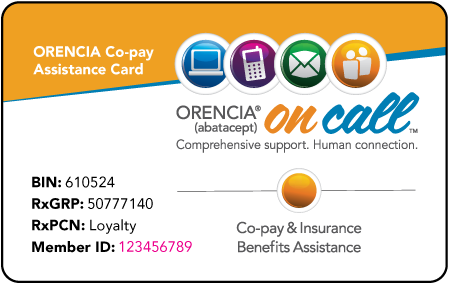
Some prescription drug plans have established programs referred to as ‘co-pay maximizer’ programs. Eligible patients with an activated co-pay card and a valid prescription may pay as little as $5 per 30-day supply monthly, annual, and/or per-claim maximum program benefits may apply and vary from patient to patient, depending on the terms of a patient’s prescription drug plan and to ensure that the funds are used for the benefit of the patient, based on factors determined solely by Bristol-Myers Squibb. Patients or their guardian must be 18 years of age or older. Patients must be treated with ORENCIA for an FDA-approved indication. Cash-paying patients are not eligible for co-pay assistance. Patients who move from commercial to federal health insurance will no longer be eligible. Patients who have insurance coverage through a state or federal healthcare program, including Medicare, Medicaid, Medigap, CHAMPUS, Tricare, Veterans Affairs (VA), or Department of Defense (DoD), are not eligible. 
Co-pay assistance is not available if patient out-of-pocket expenses are $5 or less.
Orencia copay card phone number full#
Patients must have commercial insurance that pays for ORENCIA but does not cover the full cost.






 0 kommentar(er)
0 kommentar(er)
